Staphylococcus aureus. Its source and effects inside the human body.
Staphylococcus aureus facts
Staphylococcus aureus is a normal part of the skin flora. It lives and grows on all animals. Scientists are not sure why they do, but it is thought to be a part of normal body defense against pathogens. In normal amounts, they are harmless, probably useful. When in large amounts they are pathogenic. Staphylococcus aureus is abundant in the nasal passage and in wounds. It is thought that it’s presence could have a type of healing effect or pathogenic prevention effect, in these areas of the body. In other areas this amount of S aureus is pathogenic.
That is why you should not sneeze on food. The snot is harmless, but you just put a lot of Staphylococcus aureus in the food. That is also the reason that we do not need people’s wounds dripping in our food. The blood is harmless, but you are introducing a lot of S. aureus in our food. You prick you!
S. aureus pathogenisity
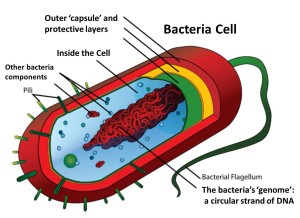
S. aureus is able to translate through the intestinal wall and enter the blood stream. In the process of growing and reproducing it creates a hemolysis through hemolase.
Let me explain this. Anything that ends in ‘ase’, is a enzyme. Enzymes break things down. Anything that ends in ‘ose’, is a sugar.
glucose – a monosaccharide in animals for energy source and storage in animals.
sucrose – a monosaccharide in plants for energy and energy storage.
lactose – a disaccharide in milk containing one glucose molecule and one galactose molecule.
Carbohydrates are broken down to glucose, the energy source in all animals. For lactose to be used in animals, it must be broken down into glucose and galactose. Lactase, an enzyme that babies produce to break down lactose, decreases with age. In some, their body quits producing lactase, resulting in lactose intolerance.
Knowing what an enzyme is now, and that it always ends in ‘ase’, tell me what hemolase, a byproduct of S. aureus growth and reproduction does in the blood stream.
If you said “breaks down red blood cells”, then you were right. Technically it lysis the cell.
This could ruin your whole day.
Article by Lisa gene Cox <*^*>