Consuming probiotics – also know as “good” bacteria – via supplements or yogurt has been popularized as a way to maintain gut health. While taking a daily dose of probiotics may not be harming you, it also may not be helping. The idea that every probiotic is good for every disease or condition is oversimplified, according to Catherine Lozupone, an assistant professor of medicine at the University of Colorado School of Medicine.
Lozupone spoke on a panel about the human microbiome, or the bacteria that reside in and on our bodies, that I attended at the Association of Health Care Journalists Conference last month. The panel touched on misconceptions related to probiotics, so I gave Lozupone a call post-conference to learn more.
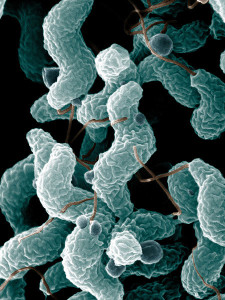
One misconception Lozupone brought up was the idea that probiotic supplements should be used for “reseeding the good bacteria” missing in a person’s gut. Probiotic supplements often only contain a few species of bacteria, whereas a healthy gut generally has hundreds of species. In addition, the microbes that are abundant in a healthy gut are often different than those found in many supplements. A healthy gut is mostly composed of bacterial species that fall within a two different groups of bacteria: the phyla Bacteroidetes and Firmicutes. One group of bacteria commonly found in probiotics is known as Lactobacillus. While Lactobacillus is a type of Firmicute, it isn’t a type of Firmicute that is typically found in great abundance in a healthy adult gut, according to Lozupone. While Lactobacillus may be helpful for some people in some situations, the idea that everyone needs to repopulate their gut with this “good” bacteria is an overgeneralization.
“I think probiotics have a ton of potential, but different bacteria are going to do different things in different contexts,” Lozupone said. “This notion [of] ‘oh just reseed the good bacteria … they’re good for you’ is definitely very oversimplified.”
But while some general probiotic health claims are ahead of the research, studies do suggest that particular types of probiotic bacteria have potential for specific uses.
For example, Lozupone noted some rodent studies suggest certain microbes might mitigate certain effects of a high-fat diet, which could be helpful to treating obesity and associated health problems.
“There’s just lots of different contexts where the microbiome has been shown to be important,” Lozupone said. Going forward, researchers hope to not only find microbes that have health effects, but also understand why they have these effects. If you’re interested in keeping track of the current research into our body’s bacteria, keep your eye on the NIH’s Human Microbiome Project, an international effort to study the role of the body’s bacteria in our health.